Zeljko Kojadinovic, MD- Neurosurgeon and Pain Specialist
Important facts about back pain:
- ANY BACK PAIN MUST BE REDUCED OR ELIMINATED. THE EFFECTS OF TREATMENT SHOULD BE OBVIOUS WITHIN A FEW DAYS.
- IT IS ESSENTIAL TO DETERMINE WHICH STRUCTURE REALLY HURTS YOU BECAUSE TREATMENT DEPENDS ON THE RIGHT DIAGNOSIS. YOUR BACK PAIN CAN HAVE DIFFERENT DIAGNOSES: DISC HERNIATION, NERVE INFLAMMATION, FACET SYNDROME, SACROILIAC JOINT INFLAMMATION, MUSCULUS PIRIFORMIS SYNDROME, MYOFASCIAL PAIN, ETC.
- DIAGNOSES OF LOW BACK PAIN AND SCIATICA ARE NOT PRECISE ENOUGH.
- DISC HERNIATION CAN BE TREATED WITHOUT SURGERY IN MOST CASES.
- THE COMBINATION AND DOSAGE OF MEDICATION MUST BE INDIVIDUALLY PRESCRIBED AND THE SAME THERAPY IS NOT APPROPRIATE FOR EVERY PATIENT. TO ACHIEVE THIS, BESIDES SPINAL IMAGES, DETAILED COMMUNICATION WITH A PATIENT IS REQUIRED TO GET ALL THE CHARACTERISTICS OF HIS PAIN.
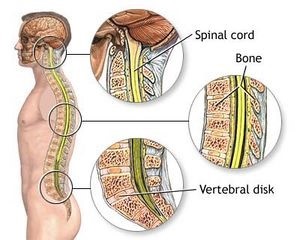
The spinal column allows a person to walk upright. It consists of 33-35 vertebrae (bone elements) between which are discs that function as shock absorbers. There are 3 parts of the spine: cervical, thoracic, and lumbosacral. Muscles are attached to the spinal column which enables various movements. Inside the spinal column, there is a canal in which the spinal cord and the beginnings (roots) of the spinal nerves are located. These nerves innervate the body.
Back pain and sciatica are very common in every population. Almost everyone has experienced at least occasional back pain. Unfortunately, there are many patients who have frequent painful phases in the back, or the pain is constant. Initial diagnosis can be chronic Low back pain (LBP), lumbar syndrome, sciatica, spondylosis, or something similar. In fact, these diagnoses are not precise at all, but in milder cases, they are sufficient to begin treatment (use of analgesics with or without physical treatment). If the pain persists despite this therapy, or recurs frequently, it is necessary to determine the exact cause of the pain. Back pain is very frequent in all countries around the world (USA, Nigeria, Kenya, Tanzania, Germany, Japan, etc.).
Causes of Low Back Pain
The cause of the pain can be one or more structures in the form of pain points (often about 1 cm in diameter). Every region of the body, especially the lumbosacral spine, has a large number of possible sources of pain (10-20 per region). For example, the same back pain in different patients can originate from about 20 different structures that usually each require specific treatment. Good knowledge of the pain anatomy makes it possible to determine exactly which structure hurts.
Low back pain can occur due to inflammation, spasm, or pressure in many tissues (e.g., muscles, ligaments, joints, capsules and attachments of these structures, nerves, etc.).
Examples of such diseases are piriformis muscle syndrome, facet syndrome, obturator nerve syndrome, other entrapment syndromes, inflammation and injuries of various back muscles, inflammation of the sacroiliac joint, nerve root diseases (radiculopathy), inflammation of ligament attachments, stretching of various ligaments, etc.
The occurrence of these diseases is associated with improper posture, obesity, trauma, and weakness of the muscles that support the spine (deep muscles around the spine). Constant pressure on the spine also contributes to their appearance (long sitting without a special cushion to relieve the spine from static loads, overweight, heavy workloads, irregular bending and lifting movements, excessive sports activities, etc.).
In particular, we must emphasize the long-term sitting of young people on chairs while working on computers (over 2 hours a day for more than several months even years). This leads to chronic static loading of certain anatomical structures in the low back end tailbone region (tailbone, ligaments, joints, muscles, nerves, and/or bursas). As a result of these loads, chronic inflammation, spasm, compression of small nerves and other types of irritation occur in them. These are the increasingly present sources of chronic pain in different parts of low back pain or the coccyx as in the illustration below. These pains could have been prevented by the application of special cushions in young people who sit for long periods of time to relieve the aforementioned structures while sitting. Precisely for these reasons, in collaboration with Penlar, we created a cushion for long-term sitting adapted to different measurements of users.

Not only did we manage to eliminate all the bad features of other cushions on the market that were not created by pain management experts, but we also added many positive features so that we could treat the pain as best as possible.
The disease can also begin in the context of various rheumatic diseases or as a result of injuries.
Spine problems are also common in diseases that attack a large number of organs, e.g., systemic autoimmune diseases, osteoporosis, some blood diseases, malignant diseases, diseases that lead to reduced movement for a long time, etc.
Many diseases of the surrounding organs can cause pain that mimics diseases of the spine (kidneys, uterus, ovaries, etc.)
Symptoms of Low Back Pain
Low back and sciatica are the most common types of pain. They can be like typical pain, but sometimes they can also be like a burning pain. Another symptom is low mobility of the spine. There can also be sensitivity symptoms (most often numbness or tingling in the foot). Muscle weakness may also occur.
Diagnosis of Low Back Pain
The task of diagnostics is to discover the real cause of low back pain, especially when it is resistant to treatment. The most important thing during the examination is to speak in detail with the patient about all the symptoms and to consider all of the above-mentioned causes of pain.
After examination, images may be indicated: X-ray, CT, and MRI of the spine, EMG, blood lab, etc. All of these images should be analyzed according to all of the symptoms the patient has. In about 50% of cases, the cause of the pain is not visible on these images. There is a possibility that one of these causes of pain could be masked by a disc herniation that can be seen on the MRI, and whose surgical removal would not lead to a reduction in pain.
Sometimes there is an indication for diagnostic-therapeutic pain procedures to find a source of the pain. One ml of local anesthetic is injected under navigation (by ultrasound, X-ray, or CT) into a suspected cause of the pain. If the pain stops, it can be the cause of the pain.
Treatment of Low Back Pain
If the source of pain and pathological process that irritates is not discovered, treatment is usually not successful or the results are not long-lasting. If the exact origin of the pain is discovered, even after a long period of pain, success is achieved in over 80% of cases.
If you suffer from persistent pain, we offer you a video consultation with our pain management expert, who will aim to precisely determine the exact cause of your pain and then prescribe the appropriate treatment. If you suffer from persistent pain, it obviously means that your doctors have not yet achieved this for you.
The above-mentioned diseases are usually not treated surgically.
Treatment can include:
- medications (different combinations and dosages should always be prescribed individually)
- special means of relieving the source of pain from mechanical irritations – special cushions for sitting adapted to the patient’s height, weight, and type of pain, losing weight, changing habits, reducing workloads, etc.
- physical therapy – traction, exercise, education, relaxation, heat, magnet, therapeutic ultrasound
- invasive treatment procedures- application of medications by injection in the sources of the pain, heat denervation.
- acupuncture
- chiropractic
- alternative methods
- surgical methods – usually spine surgery,
- implanting spinal pumps or spinal and nerve stimulators

LUMBAR DISC HERNIATION
Diseases of the lumbar spine are numerous and mostly begin with various pain syndromes. Low back pain with or without irradiation to the leg is most common. In advanced disease, and sometimes from the very beginning, there may be signs of damage to the roots (radix) of the leg nerves (radiculopathy). …
These changes are usually diagnosed on magnetic resonance imaging of the lumbar spine and are usually located in the lower part of the spinal canal….
>> FULL TEXT about tarl cysts
Spinal diseases in the elderly
Most people over the age of 60, 70, and especially 80 suffer from back pain. This pain is often intense and long-lasting and makes their daily activities significantly more difficult. In addition to this, they often have associated diseases. ……
>> FULL TEXT on spinal diseases in the elderly
Patient questions
These are some frequently asked questions. Maybe you have similar problems?
- Findings of an MRI of the lumbar spine indicate moderate degenerative changes of the type of spondylosis on bone structures, minor Schmorl herniation of the upper surface of the L3 vertebra, and disc bulging at the levels L4-L5 and L5-S1. Can you explain to me exactly what of above-described changes is a cause of my sciatica? Grateful in advance.
Answer
The most important thing is to find out the cause of your pain. This MRI shows many pathologies but they probably aren’t the cause of your pain. Most causes of pain are not detectable by MR imaging. I think you need to contact an experienced pain specialist who will first analyze all the specifics of your pain in detail.
- I have had pain in the lower back for more than half a year that spreads to the hips and down the left leg to the foot. The MRI finding is as follows: at the level of L5-S1, a disc herniation is present on the left, with radicular compression and compression of the dural sac and stenosis of the spinal canal. The neurologist advises surgery and I am interested in your opinion. I don’t use therapy. Thanks in advance.
Answer
Treatment of most disc herniations does not require surgery. However, it is best that the decision be made by a neurosurgeon. He will tell you if surgery is needed immediately or if other methods of treatment can be ordered first (which is usually possible). Finally, it is important to diagnose if there are other sources of pain besides disc herniation and to inform you of the probability of part of the pain remaining after the operation and how it will be treated further. After disc herniation surgery some pain lags behind in 25% of cases.
More about back pain- here

