Zeljko Kojadinovic, MD- Neurosurgeon and Pain Specialist
There are over 80 types of tumors that can grow inside the skull and lead to brain damage. However, in adults, 5 types of tumors occur in over 90% of cases. They are:
- Gliomas – these include astrocytomas, oligodendrogliomas, anaplastic astrocytomas, glioblastoma, and more.
- Meningioma
- Neuroma, schwannoma- mostly on the acoustic (vestibular) nerve
- Pituitary adenomas- hypophysis tumors
- Brain metastases from distant malignant tumors
Causes of Brain Tumors
These, as well as other tumors in the body, occur due to changes (mutations) in special genes of normal cells. By mutation, some genes become active (proto-oncogenes become oncogenes), and others are inactivated (tumor suppressor genes). This happens continually in the body in many cells, but the immune system recognizes these cells and neutralizes them. Sometimes these cells are not neutralized and, if they continue to multiply, a tumor is formed from them. It is usually benign at first, but over time it can accumulate an increasing number of these genes and so the tumor can become more malignant.
The reasons for these gene changes are not always known. Mutations can be the result of the action of some viruses, which have previously caused minor infections; radioactive radiation; or some chemicals (there is growing proof that various pesticides and even food additives can be carcinogens). Almost no brain tumor is directly inherited, but the offspring of people who have had malignant diseases may have inactivated proto-oncogenes, or a weaker immune system, etc. However, the influence of some factors, such as radiation from mobile phones (especially on children), radiation from high-voltage electrical cables, frequent X-rays, some medications, head injuries, poor diet, etc., are still being investigated.
Types of Brain Tumors
These tumors, according to how quickly they progress and in what percentage they can be cured, are divided into benign and malignant tumors. Meningiomas, neuromas, and pituitary adenomas are usually benign. Metastases are always the result of malignant disease, and gliomas are more often than not malignant. One type of glioma – glioblastoma – is the most common malignant brain tumor.
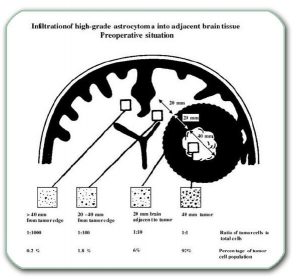
According to their growth, tumors can be divided into those that, as they grow, only press on the surrounding parts of the brain, those that infiltrate the brain, and combined ones (e.g. larger malignant tumors infiltrate the brain and put pressure on it).
The mechanisms by which the tumor damages nerve tissue are numerous and interconnected. When the tumor reaches a significant size, it puts pressure on the brain. It also causes nervous tissue to swell, disrupts blood flow in the nerve tissue, and can lead to bleeding.
Symptoms of Brain Tumors
All this brain damage causes symptoms such as: headache, epilepsy, drowsiness, various impairment in the function of the brain and nerves of the head. Malfunction depends on the location and size of the tumor. There can be the following deficits in: vision, speech, hearing, smell, limb movement, balance, touch, mental disorders, etc. In benign tumors, one or more symptoms appear first, and then for months, and often years, although the tumor continues to grow, new symptoms do not occur. The symptoms, due to slow growth, appear only when the tumor grows significantly.
Diagnostic Workup of Brain Tumors
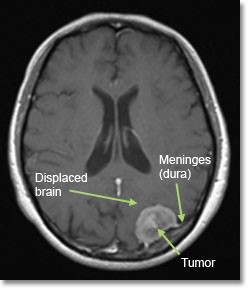
Since small tumors are much easier to treat than large ones, it is important to diagnose them as soon as possible. The most important diagnostic method is magnetic resonance imaging (MRI) of the brain. Thanks to widespread availability, this recording should be done at the first symptoms that indicate that there may be a tumor. So any perceived deafness, epilepsy, odor or vision disorder, psychiatric disorder, etc. should be considered sufficient reason to order a brain MRI. This recording is painless and lasts about 15-45 minutes. It involves the patient lying in the narrow space of a device and being exposed, to a greater or lesser extent, to noise. This can be so uncomfortable for some people that it must be done under sedation or anesthesia (through previous administration of tranquilizers or sleeping pills). Usual intravenous contrast (non-iodine contrast) should be administered.
In addition to this, other diagnostic methods can be indicated, such as: computed tomography (CT), electroencephalography (EEG), various types of evoked potentials, endocrinological tests (hormone tests), vision and hearing tests, bone imaging after administration of radioactive substances (skeletal scintigraphy), etc.
Imaging of other organs (oncological treatment) must always be done to investigate the possible existence of other tumors in the body. It is also important to determine if the patient is suffering from other diseases. This can be important when planning anesthesia and choosing treatment methods. Minimum testing requirements are: laboratory processing of blood and urine, ECG, X-ray of the lungs, ultrasound of the abdomen and examination by an internist. Additional examinations can be performed if necessary: urological, cardiological, gynecological, etc.
Treatment of Brain Tumors
When a brain tumor is diagnosed, a team of experts (a neuro-oncology team) considers possible courses of treatment for the patient. We have at our disposal: symptomatic, surgical (tumor surgery) and adjuvant treatment. The decision on how to treat a patient is made based on knowledge and experience in neuro-oncology.
In some cases, there are indications that the tumor has finished growing and does not interfere with brain function. In that case, especially in the elderly and people who are more seriously ill with other diseases, we decide to only monitor the tumor (through periodic MR or CT scans).
Symptomatic treatment is carried out in case of brain swelling, headache, epilepsy, vomiting, etc. For brain swelling in tumors, the corticosteroid Dexamethasone is most often prescribed. It is given as an injection or, less commonly, as tablets.
Surgical Treatment of Brain Tumors
Surgical treatment involves opening the skull (craniotomy), accessing the tumor and removing it. During removal, the surrounding structures (nerve tissue, nerves, blood vessels) must be separated from the tumor. This is impossible if the tumor has infiltrated them (grown infiltratively). This is the case with most gliomas, as well as with aggressive and malignant variants of other tumors. If a benign tumor grows for a long time and becomes large, it compresses, thins and strongly adheres to the surrounding structures. It is then often impossible to separate the tumor from surrounding structures while fully preserving their function. This is the main reason why it is important to arrive at a diagnosis early, while the tumor is smaller in size.
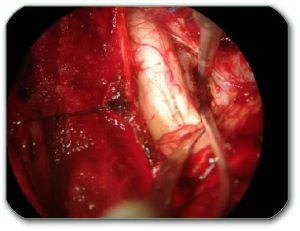
Depending on whether the tumor can be separated safely from the surrounding structures, it will be either completely removed or merely reduced in size. In the case of reduction, usually only a very small portion of the tumor remains. In order for the treatment to produce optimal results, it is important that the operation is performed by a surgeon who has extensive experience in such operations, has an excellent technique of operating under a microscope and constantly introduces new surgical methods into his routine. These methods make his surgical work easier and make him more precise and safer. These methods are: more detailed diagnostic processing before surgery; the use, during surgery, of an ultrasound scan of the brain to see exactly where the deep tumor is located; other methods of neuronavigation; recording the functions of nerve structures during surgery (neurophysiological monitoring); Ultrasound tumor aspirator (CUSA), etc.
In some cases, when the risk of surgery is high, only tumor samples (biopsies) are taken during the operation. This can be done stereotactically.

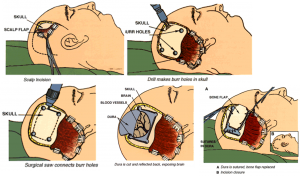
The results of surgical treatment depend mostly on: type, malignancy, size and location of the tumor. Surgery-related mortality is generally less than 1% and is usually caused by worsening of other diseases. The neurological damage caused by the operation depends on the size and location of the tumor. Generally it tends to occur in less than 1% of cases. In more severe localizations and larger tumors, neurological damage after surgery occurs in 20% of patients. It is important that the possible damage from different types of operations (complete removal or only reduction of the tumor) is communicated in advance to the patient and his relatives.
The pathohistological (PH) analysis identifies the type of tumor and its degree of malignancy. It needs to be done a few days after surgery. PH analysis consists of preparations of tumor tissue sections with special stains, which are then examined by a pathologist under a microscope. We then decide whether additional treatment with radiation and/or chemotherapy is needed.
Adjuvant Treatment of Brain Tumors
Adjuvant treatment methods are radiation and chemotherapy.
Radiation therapy is most often performed using radiation devices that have different degrees of precision. Standard radiation therapy is performed in multiple sessions (30 to 70), irradiating through different parts of the brain each time. This way, the tumor receives by far the highest doses of radiation (dosage is measured in Grays – Gy). The most precise radiation is achieved by using radiosurgical methods (Gamma knife, Linac, cyber knife, etc.). Such precise radiation can stop the growth of tumors if they are no larger than 2.5-3.5 cm in diameter and are not very close to brain structures that do not tolerate radiation. They can also stop the growth of smaller parts of the tumor that are left behind after the operation. Mostly single radiation is sufficient.
Today, chemotherapy usually involves the use of temozolomide (Temodal, Temodar). It is a drug that is taken in the form of tablets and has fewer side effects than other cytostatics.
We believe that these types of treatment do not exclude many alternative methods of treatment. We are generally not against them. These methods should always be discussed with experts. This is not to discourage the patient from trying them, but to prevent alternative therapists from affecting the results of classic medical therapy. There have been instances where the alternative therapist makes changes to the primary treatment, administers treatment that the patient has already received, or promotes drugs or substances that have not been clearly shown to be effective or even some that are harmful.
Specific tumor types
If you have been given a neurosurgical diagnosis and suggested operative or non-operative treatment, you can consult us if you have any doubts. This will make it easier for you to accept the proposed treatment from your doctor and, since you have no doubts, the treatment will have a better result or you will opt for a different type of treatment. We will explain whether we think surgery is indicated, which operative methods exist, where in your country such surgeries are performed, what their risks are and how to reduce them. We will also answer all your questions.
Gliomas
Gliomas originate in the glial cells that surround and support neurons in the brain, including astrocytes, oligodendrocytes and ependymal cells. Their names are astrocytoma (the most frequent and usually more malignant), oligodendroglioma and ependymoma (usually located at brain ventricles, less invasive than the other types). Most often, during growth, they infiltrate the surrounding brain structures. They have great potential to become malignant. Depending on the degree of malignancy, they have 3 or 4 stages. In the first stage, a cure is very likely. In the second stage, the 5-year survival rate already drops to 50-80% of cases. In stages 3 and 4, the odds of survival are even lower. After the operation, radiation is always performed and chemotherapy is often indicated. Some tumors, such as oligodendrogliomas, respond better to chemotherapy, while others, such as ependymomas, respond better to radiation. Causes, symptoms, diagnostic, surgery and adjuvant treatment are explained in the first part of this page. Generally, astrocytomas have a worse and ependymoma have a better prognosis. With the development of oncogenetic new modalities in diagnosis, prognosis and treatment are available. Knowledge of new prognostic parameters allows doctors to recognize patients with a better prognosis even if they are at 4th PH grade malignancy. These patients should be treated more aggressively.
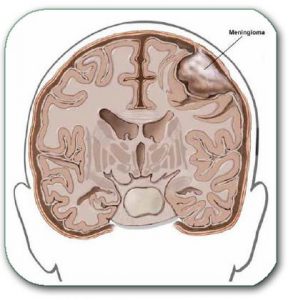
Meningioma
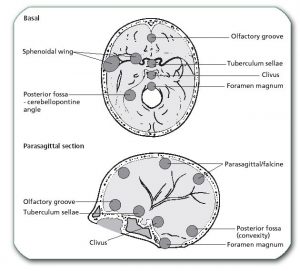
Meningiomas are, in most cases, benign tumors. They grow from the meninges (membranous coverings of the brain), pressing on the surrounding parts of the brain, nerves and blood vessels. They often cause significant brain edema. If they are not firmly attached to the brain, nerves and arteries, they can be completely removed. Meningiomas can grow on different parts of the skull (above the cerebrum, above the cerebellum, on different parts of the base of the skull). The problems and deficits they cause depend on the size and location of the meningioma. (A large number of, quite different, clinical pictures are listed above). The diagnosis of meningioma is then Meningioma + the name for localization (olfactory, sphenoid medial, sphenoid lateral, tuberculum sellae, sinus cavernosum, clival, petroclival, foramen magnum, pontocerebellar angle, convexity, sagittal, parasagittal).
Its growth, diagnosis and treatment are explained in the introductory part of this page.
It is important to arrive at a diagnosis while the tumors are still small.
There are also malignant variants – atypical meningioma and meningiosarcoma.
When a tumor in the skull is diagnosed on MRI, there are a large number of indicators that indicate that it is a meningioma. Neurosurgeons need experience to decide whether to operate on the patient, or to just monitor the tumor. We usually decide on monitoring when we think that the tumor does not create increased pressure on the surrounding structures, and that it has finished or slowed down with growth. This is especially true in the case of elderly patients or patients who are seriously ill due to other diseases.
Fortunately, with good surgical technique, it is possible to completely remove the vast majority of meningiomas without major neurological damage (especially if the tumor is not large and has a favorable localization). Causes, symptoms, diagnostic, surgery and adjuvant treatment are explained in the first part of this page.

Neuroma and Schwanoma
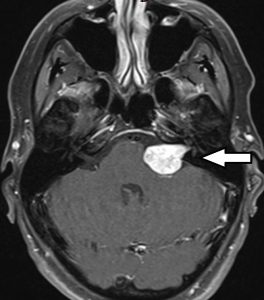
Acoustic neuroma, also known as vestibular schwannoma (the more precise name), is formed from cells located in the nerves. They are most often localized on the nerve for hearing and balance. Because of this, they usually start with hearing loss and dizziness. These symptoms may remain the only symptoms for years. Later, when they grow bigger, they can cause tingling and pain in the face (symptomatic trigeminal neuralgia), facial palsy due to facial nerve damage, weakness of the extremities due to pressure on the brainstem, or hydrocephalus (accumulation of brain fluid in the brain chambers).
It is important to diagnose tumors while they are still small.
When a tumor in the skull is diagnosed on MRI, there are a large number of indicators that indicate that it is a neuroma. Then we need experience to decide whether to operate on the patient, or to just monitor the tumor. We usually decide to follow up when we think that the tumor does not cause increased pressure on the surrounding structures (brain stem, surrounding nerves, cerebrospinal fluid pathways), and that it has finished or slowed down with its growth. This is especially true in the case of elderly patients or patients who are seriously ill due to other diseases.
It is usually possible to remove them completely. An alternative to surgery, especially in small neuromas (<3cm in diameter), is stereotactic radiation (e.g., Gamma knife).
Pituitary tumors
These are tumors that grow from a single gland with internal secretion. This gland is located below the middle of the brain, and above the nose. These tumors can secrete more hormones and in such cases are usually diagnosed earlier, while they are still small. Depending on which hormones they secrete, the patient will develop hyperprolactinaemia, Cushing’s disease, Acromegaly, or, less frequently, other hormonal disorders. If it does not secrete the hormone, the tumor grows quiet until it shows the first symptoms of compression of the optic nerves. Large adenomas usually manifest first as a visual impairment. Later, the following may occur: decreased secretion of pituitary hormones, ventricle dilatation, double vision, frequent urination, difficulty walking, mental problems and signs of hydrocephalus.
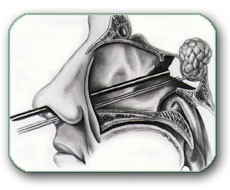
Some smaller tumors (usually prolactinomas) are treated with medication. Most pituitary adenomas today can be removed by surgery through the nose, without opening the skull. For tumors that grow aggressively, radiation therapy is also a possibility.
Most operations through the nose today are performed using an endoscope. By these methods (“through the nose” without opening the skull) a large number of skull-based tumors can also be removed. In order to perform these operations, in addition to endoscopy, a range of other equipment is needed, such as navigation, neurophysiological monitoring, etc. For big adenoma sometimes opening the skull (craniotomy) is indicated.
After surgery on pituitary adenoma, the surgical result is evaluated on a follow-up brain MRI and hormone serum analysis. Also additional treatment by an endocrinologist is usually required.
Brain metastases
If there is a malignant tumor in the body, malignant cells constantly separate from it and travel through the bloodstream. They can then start to grow in various organs (most often in the lungs, liver and brain). The most common metastases within the brain come from a malignant tumor (cancer) of the lung (40% of all brain metastases), breast cancer, melanoma of the skin, kidney cancer, gastrointestinal cancer, prostate cancer, etc. Brain metastases can usually be completely surgically removed. In a situation of multiple brain metastases that are remote from each other, deeply placed and/or do not have a large diameter, and small cell lung carcinoma is also present, only radiation and/or chemotherapy can be performed. If the patient’s general conditions very severe, and they are in the terminal phase of the malignant disease, only symptomatic treatment is indicated.
Causes, symptoms, diagnostic, surgery and adjuvant treatment are explained in the first part of this page.


Brain tumors in children
After leukemia, these are the most common tumors in children (20%). The most common are: gliomas (especially astrocytomas of the optic nerve, brainstem and cerebellum), medulloblastomas (and other PNET tumors), pineal tumors, craniopharyngioma, plexus papilloma and teratoma. Cerebellar tumors are much more common in children than in adults (42-74%, depending on the age of the child).
More about brain tumors – here

